For the past 100 years when people were not well, they called their doctor on the telephone and been given advice or an appointment. With the advent of the internet, most people now seek online healthcare advice. Patients use patient portals for everything and want access to their doctor’s office via the internet. Online care now exceeds those who want to call on the telephone. Therefore, the internet needs to become the dial tone of the 21st century medical practice for most patients. There will always be technically challenged individuals, but they can receive help from family or friends.
When the Patient Contacts a Patient-Centered Office
In today’s healthcare systems, processes are designed to treat illnesses efficiently and maximize profits, often prioritizing provider utilization over patient needs. For example, highly paid doctors have schedules booked far in advance, making their availability scarce. In contrast, a patient-centered office focuses on aligning schedules to fit the patient's needs, keeping time free for necessary care rather than maximizing the provider’s billings.
In a patient-centric model, the office schedule remains open until patients reach out. By filling most appointments on the same day the patient calls allows for flexibility in addressing care promptly. Receptionists in this setting work closely with the clinical team and are often dedicated to specific doctors or small provider groups. This structure fosters familiarity with the doctors' preferences for visit durations and common processes. It also helps staff recognize frequent patients and tailor care accordingly, offering a stark contrast to the impersonal approach of large receptionist pools tasked solely with filling appointment slots far into the future.
Streamlined Patient Interaction
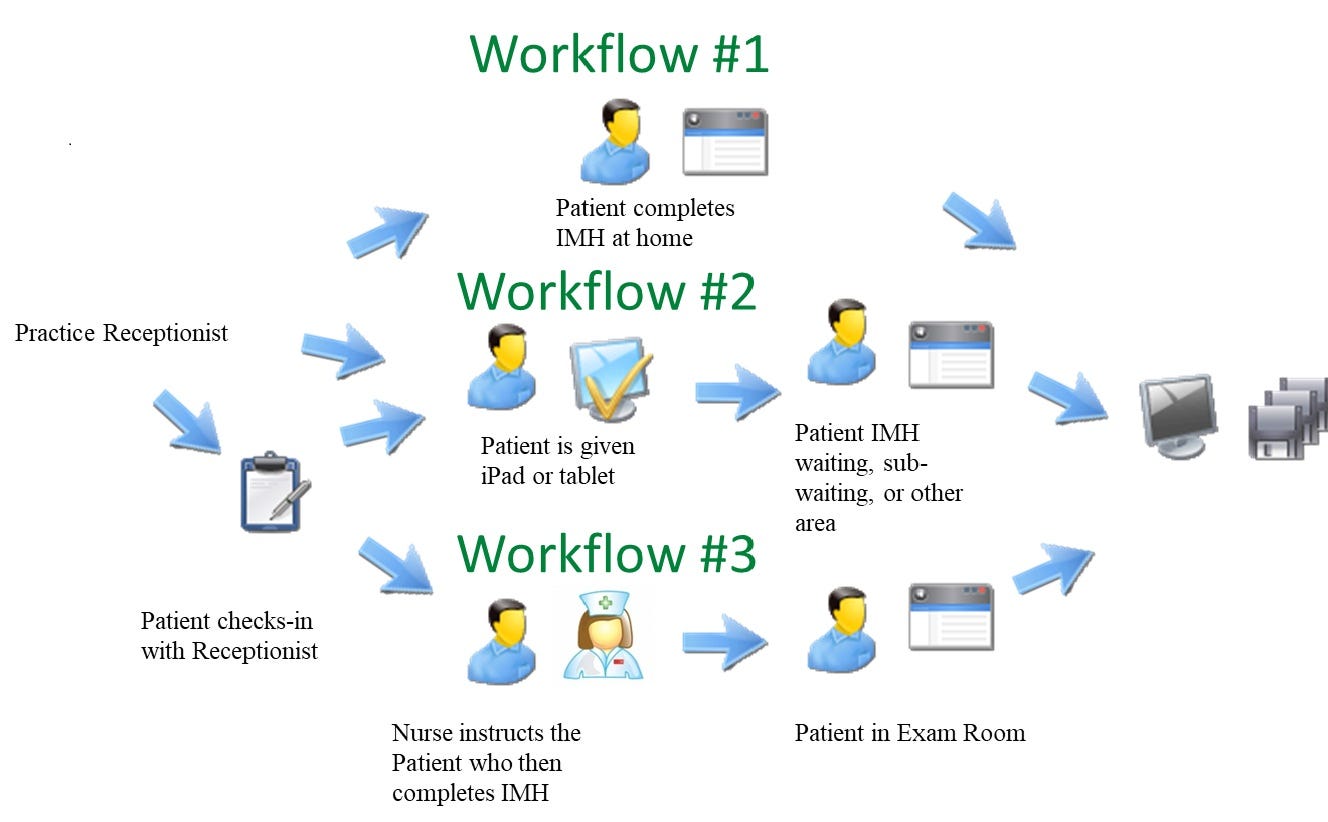
When patients contact a patient-centered office, the receptionist, who is medically trained, triages and prioritizes care. Patients are asked about their access to digital tools like smartphones, tablets, or computers. Instead of scheduling an appointment immediately, they are guided through a pre-visit process. If they have access, they can go directly to the practice website, or receive a hyperlink via text/email and complete an online interview often on their smartphone.
For the 7% of patients without internet access, they are either placed on hold for a staff member to conduct the clinical interview, or, if well-known to the staff, they are simply given an appointment time 30 minutes earlier than the time recorded in the schedule. These patients simply complete their computer interview in the waiting room.
For instance, at Trillium Family Practice in Asheville, N.C., Dr. Mark McNeill has been using a tech-driven approach for over a decade. Most patients use the internet instead of calling. They complete a web-based pre-visit AI interview [that informs the scheduling process.1[1] The initial questions address conditions requiring immediate hospital visits (e.g., blindness, syncope, seizure) and advise the patient to seek emergency care. Once the online interview is completed, an appointment is scheduled within two hours. This process gathers comprehensive clinical information beforehand, ensuring the care team can prioritize and address the patient's needs effectively. The staff has detailed information about the reason for the visit, understands the urgency of the problem, knows what tests or measurements will be needed before the visit, and exactly how much time to allocate on the schedule. As a result, the doctor’s day runs smoothly for patients, staff, and doctors, leaving the waiting room empty and the entire office quiet.
Leveraging Technology for Efficiency
The interview process utilizes adaptive software, similar to the logic of a clinician’s inquiry. For instance, if a patient reports urinary symptoms, follow-up questions delve into duration and severity. The artificial intelligence of the software translates answers to questions into medical terminology. This data populates the medical record as digital information but also generates a human-readable detailed medical history formatted like a traditional medical record. Trained clinical staff can glance at the results and decide quickly what to do for the patient. Note that the AI of the system also provides clinical decision support from the medical literature to make the clinicians job easier.
Proactive Care Decisions
The clinical team reviews the patient documentation to determine the urgency and type of care required. There are several outcomes which depend on the type of condition as described by Clayton Christensen2 and discussed in Case #1 Episode #9, Which Provider Do You Need? . The office knows from the pre-visit information what type problem the patient has:
1. Value Healthcare complaint
Conditions like influenza, sinusitis, female urinary tract infection, and seasonal allergies have known signs and symptoms, a known diagnosis, a known treatment, a known outcome. After review of the data by the doctor, the patient would receive a call, text or email from the doctor or nurse and be instructed on what to do or to go to the pharmacy. For example, a patient with an initial occurrence of a urinary tract infection may receive a call from their doctor to discuss treatment options without needing a visit. If the symptoms recur, a face-to-face appointment might be scheduled for further evaluation to identify underlying causes. This would have been the likely scenario in Case #1, the 24-year-old female with urinary discomfort. Here is a video of the actual interaction.
2. Network healthcare complaint
Conditions like high blood pressure, diabetes, asthma, arthritis, and chronic lung disease have already been diagnosed and a long-term treatment plan is underway. For example, suppose the information about a patient with high blood pressure is shown to be controlled with no new symptoms like headaches or chest pain. The patient could receive a refill of the medication sent to their pharmacy without a face-to-face visit. Follow up could again be virtual until an annual in-person exam. A call, text or email would be all that was needed. If a medical side effect were identified or the condition was not controlled, they could be scheduled for a same day visit or the medication changed. The process could be repeated with a follow-up in 2 weeks
3. Solution healthcare
Some conditions like fatigue, rectal bleeding, high fever, syncope (fainting), chest pain, abdominal pain, or unexplained weight loss are difficult to diagnose and treat. The problem may be simple or complex, i.e. rectal bleeding may be hemorrhoids, but it could be rectal cancer. Each of these conditions needs the attention of a skilled licensed practitioner. The patient would be given a same day appointment without delay.
This approach ensures personalized, efficient, and timely care, reflecting the essence of patient-centered practices.
Preview
Next, we will explore how a skilled clinician can replace a wide variety of tests and investigations by listening to the patient.
Christensen, C., Hwang, J. and Grossman, JH. The Innovator's Prescription: a Disruptive Solution for Health Care. New York: McGraw-Hill, 2009